Last time I wrote about getting my feeding tube (PEG tube), and I ended up being admitted to hospital for complications and observation. This post is a continuation of that post, and it picks up the story on the morning after the procedure.
Warning: more non-sugar-coated descriptions, and a photo of the finished product that some sensitive users might find unsettling. If these things bother you, please don’t read any further.
I woke up on the day after the procedure still in great pain, but it had eased enough so that I had an appetite — after all, I hadn’t eaten in a day and a half. I was delighted to see that a breakfast tray with tea had arrived, and not so delighted to see jello. I was even happier to see that Seaghan had arrived, and with him were fresh clothes and toiletries. I didn’t even get to enjoy my tea before the Gastroenterologist and an intern showed up to assess how I was doing.
I was scheduled for my third radiation treatment and my first chemo treatment that day, but the Doctor informed me that, until I was discharged from the hospital, I would not be accepted for cancer treatment. His hands were tied. I was astonished to learn that the cancer-centre policy dictated that I could not be an inpatient at the hospital. What utter rubbish! Are they not one-and-the-same institution??
The doctor and intern then examined the feeding tube and left. Seaghan decided to go to the cancer centre to see if he could get the chemo session rescheduled because I wasn’t really fit to leave the hospital just yet. Shortly afterwards the intern returned alone, and said that my tube was too loose and he needed to tighten it. Remember that I was still in excruciating pain, and he wanted to adjust it. I couldn’t even tolerate the sheet touching it, let alone have someone move it. He called for more pain killers, but decided to tighten it anyways before they could take affect.
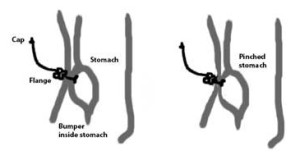
And while my hands held on to the bedside rails with a death grip that not even Hades himself could release, he tightened it. He pulled on the tube so that more of it came out of the stomach and then he tightened the flange so that there was less space between the stomach bumper and the flange. I whimpered and sobbed, and I remember that the room was deathly silent afterwards. The other patients and nurses in the room didn’t make a sound. I think they pitied my suffering, and believe me when I say I’m not exaggerating my pain. It was the most unbearable thing I have ever, EVER, gone through.
When Seaghan returned he found me still weeping, and I was further disheartened to hear that he hadn’t had any luck. There was no choice now — I had to go for my treatment or risk missing it entirely. I asked to be discharged because I strongly felt that I couldn’t afford any delays in treatment.
At this point the bloody discharge going into the drainage bag had all but stopped and the ultrasound on my abdomen that was done in the middle of the night showed that there was nothing wrong from surgery. They felt that the blood in the drainage bag that they had been worried about had come down the esophagus from the tumour down into the stomach and not from the procedure itself, so they agreed to release me. I was discharged, put into a wheelchair, and taken to the cancer centre. I swear that the wheelchair had four square tires, and every bump, no matter how insignificant they were, made me feel as though I was being punched.
I reported in at my radiation unit for my third treatment. It took Seaghan and two radiation therapists to transfer me from the wheelchair to the treatment bed, and then back again. While I was there the dietician who had arranged for my procedure decided to swing by to see how I was doing. She was astonished to find that, not only was I still in great pain, the nurse in the hospital who had released me had failed to remove the drainage bag and replace it with a proper stopper tip. A blistering phone call was made to the nurses’ station who had tended to me overnight, while a cancer centre nurse fixed the feeding tube. Once that was rectified I then proceeded to the chemotherapy reception area.
And woe is me, I was too late. My chemo session would take six hours, and it was already 3:00 p.m. They couldn’t possibly do it then; BUT, being the wonderful people that they are, they managed to squeeze me in two days from then. I would receive my first chemo session only two days late, and I was still on track with my radiation treatments.
In the mean time, Seaghan realized that he would not be able to get me out from the car, up the front steps, into the house, and up more steps to the living room without help. My neighbours were too elderly to ask for their help, or had bad knees/hips and were unable to help. My younger sister Gail to the rescue! She drove two hours from her house to my house, helped Seaghan get me out of the car (not easy to do) then into the house, then drove home again. She didn’t even want to trouble us for a coffee or tea. I was settled onto the sofa and given a cup of tea.
At bed time, I had to wrap my arms around Seaghan’s neck so that he could gently lower me down to the pillow. I needed this help getting out of bed as well, and also for lying on the sofa, getting into the car, getting onto the treatment beds, going to the washroom, and you get the idea. Basically I needed help for everything.
For the next two weeks I had to use a wheelchair when getting from the car to my treatments because I could only walk a very short distance. Every time my tummy rumbled my stomach would spasm. The pain persisted and had not subsided, and I needed hydromorphone often. The Gastroenterologist had gone on vacation, and so we couldn’t consult with him.
Finally the dietician, who’d been closely monitoring me because this whole situation was not the norm, talked the Oncologist into trying to help me. When they looked at it closely they noticed that the flange was cutting into my skin, which means that it had been adjusted too tight (curse that intern!!! Lesson learned: I won’t trust an intern again, especially if the Doctor himself didn’t say it needed fixing just after being examined.) The stomach itself and the abdomen wall were being constantly pinched together. After examining it further they figured out how to loosen it and then suddenly the pain was all but gone!! (image the hallelujah choir being sung here!!). Instant heroes!
After that, there was residual soreness which was to be expected but I could walk again. I could move again. I could sleep better. Life was good.

—Sandi
Next time: my first chemotherapy session
It’s no wonder you were in pain from the feeding tube, how horrible. In addition to the night nurse I hope they also gave the intern hell for tightening the tube. Kind of makes me wonder how many others he did that to, and if he should be doing any adjustments without a doctor present.
He told me that it was better to do it now, rather than wait and do it after it had loosened due to weight loss. I shouldn’t have allowed it to happen.
Haha thanks for graciously “forgetting” the head thump i gave you trying to put the car seat in the upward position! I still feel bad adding to what was a nightmare at the time.
As for the intern, i hope they told him about his error!
No worries about the head thump — it gave me a much-needed chuckle!
No one should have had to endure that. I’m sure the intern thought he was doing the right thing, but his ‘work’ should have been examined by a more senior health professional. Shame on them!